Introduction
Do you suffer from digestive symptoms such as cramping, abdominal pain, bloating, gas and diarrhea and/or constipation? You may have Irritable Bowel Syndrome, commonly referred to as IBS.
IBS is defined as a functional disorder, meaning that despite no obvious medical abnormality, the person has digestive symptoms. These symptoms may include:
- Chronic constipation
- Diarrhea
- Alternating constipation and diarrhea (swinging bowels)
- Bloating
- Abdominal cramping and pain
- Excessive gas
- A sense of incomplete bowel evacuation
- Nausea
- Relief after defecation
- Straining at defecation
- Sense of urgency
- Passage of mucous
There is no one cause, rather there are many contributing factors:
Dysbiosis
The trillions of bacteria that reside in your gut need to be in a delicate balance. Dysbiosis is the term used to describe when there are more “bad bugs” than “good bugs.” This can lead to activation of the gut immune system, low-grade inflammation, altered gut motility, increased permeability of the intestine and changes in the gut-brain axis. All these can cause or exacerbate gut symptoms and contribute to IBS.
Multiple food sensitivities
Food sensitivities or intolerances are considered one of the fastest growing chronic diseases which affects more than 20% of the population in industrialised countries. Exposure to food antigens can trigger rapid gut inflammation leading to barrier hyperpermeability and IBS. With food sensitivities, symptom onset is often delayed by many hours and an individual is usually reactive to a number of different foods.
Lack of digestive enzymes or stomach acid
Not having enough stomach acid or digestive enzymes means you’re not able to break down and absorb your food properly, leading to fermentation, inflammation and irritation of the gastric lining.
Low grade inflammation
Individuals with IBS have increased expression of inflammatory markers in the body, which suggests that low-grade inflammation is present. Mild inflammation of the gut lining has the ability to disrupt gut motility.
Altered GIT motility
We should experience smooth, wave-like contractions of our bowels to help move the contents through our gut, allowing it to be digested and absorbed properly. Being constipated shows that our gut motility is under-functioning and diarrhea is a sign of more rapid gut motility. Dysbiosis and low-grade inflammation can affect gut motility as well as Small Intestinal Bacterial Overgrowth, gastroparesis, medication side effects and hypothyroidism to name a few.

Visceral hypersensitivity
This refers to an enhanced intestinal perception of pain whether it’s due to underlying dysbiosis or low-grade inflammation. When you feel bloated, this may exacerbate the pain and discomfort due to inflammation and hypersensitivity.
HPA axis dysfunction
This refers to the glands and organs in your body that help to manage the stress response. Chronically elevated stress hormones impact your digestion by reducing digestive enzyme function, disruption GIT motility and causing dysbiosis.
Parasite infections
Parasitic infections such as Blastocystis hominis (BH) and Dientameoba fragilis can also lead to IBS. In fact, BH has been found to be as high as 70% in individuals with IBS.
SIBO
SIBO is where abnormally large amounts of commensal bacteria reside in the small intestine which can cause symptoms such as abdominal discomfort, bloating, diarrhea, constipation, nausea and intolerance to certain foods. SIBO has been found in 70% of patients suffering with IBS and can often be triggered after a bout of food poisoning or acute gastroenteritis.
If you suspect IBS, start with these steps to begin to build a clearer picture:
1. Get a clear symptom picture
Keep a food diary for two to three weeks so you can become better acquainted with the symptoms you experience and so you can start to draw correlations between the symptoms and the foods you are eating. After a couple of weeks, you may be able to identify patterns. It helps to be really specific about what kind of pain you are feeling (i.e. cramping, burning, bloating etc) and what your stools are like too.
2. Reflect on the stress in your life
Be honest with yourself about your stress load. How does stress manifest to you? Do you feel heart palpitations, hyper-active, tightness in your stomach or digestive symptoms? What are your triggers? Do you have strategies in place to help you cope with your stress?
3. Perform a bowel transit time test
Transit time is how long it takes from the time you ingest your food to when it comes out the other end. The ideal transit time is between 21 and 24 hours. Use corn kernels or beetroot (you’ll be able to see the corn in your stool and beetroot will make your stools purple) and time how long it takes from when you eat it to when you notice it in your stools. If it’s more than 24 hours, you have slow transit time and there is likely to be some level of constipation. If your transit time is less than a few hours and your stools are watery, you’ll know you have some level of diarrhea.

So what can you do about it?
Fortunately, there is a lot you can do to help manage IBS and reduce your symptoms. By reducing inflammation, restoring your gut microbiome, improving gut motility and incorporating some stress management strategies on a daily basis, you can reduce your symptoms and heal your gut. Here are some essential steps when it comes to treating IBS:
1. Remove the drivers that are triggering your symptoms
Now everyone is different and determining what foods you’re reacting to is important. Food intolerance testing is helpful to determine specific sensitivities however, many people do benefit from doing a low FODMAP diet. FODMAP is an anacronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. FODMAP-containing foods are a normal part of the diet, and do not cause symptoms in most individuals. However, they are a group of sugars which may be difficult to digest if you have IBS. They are osmotic, meaning they attract water into the bowel and are poorly absorbed in the small intestine, which then leads to symptoms of IBS such as bloating, gas and diarrhoea. People with IBS often show significant improvement when they avoid these foods.
If you answer yes to the following questions, then you may benefit from doing a low FODMAP diet:
- Do your symptoms worsen if you eat a lot of garlic or onions?
- Have you tried a probiotic and it made you feel worse?
See our resource on FODMAPs to find out how to implement the FODMAP diet.
2. Balance your gut microbiome
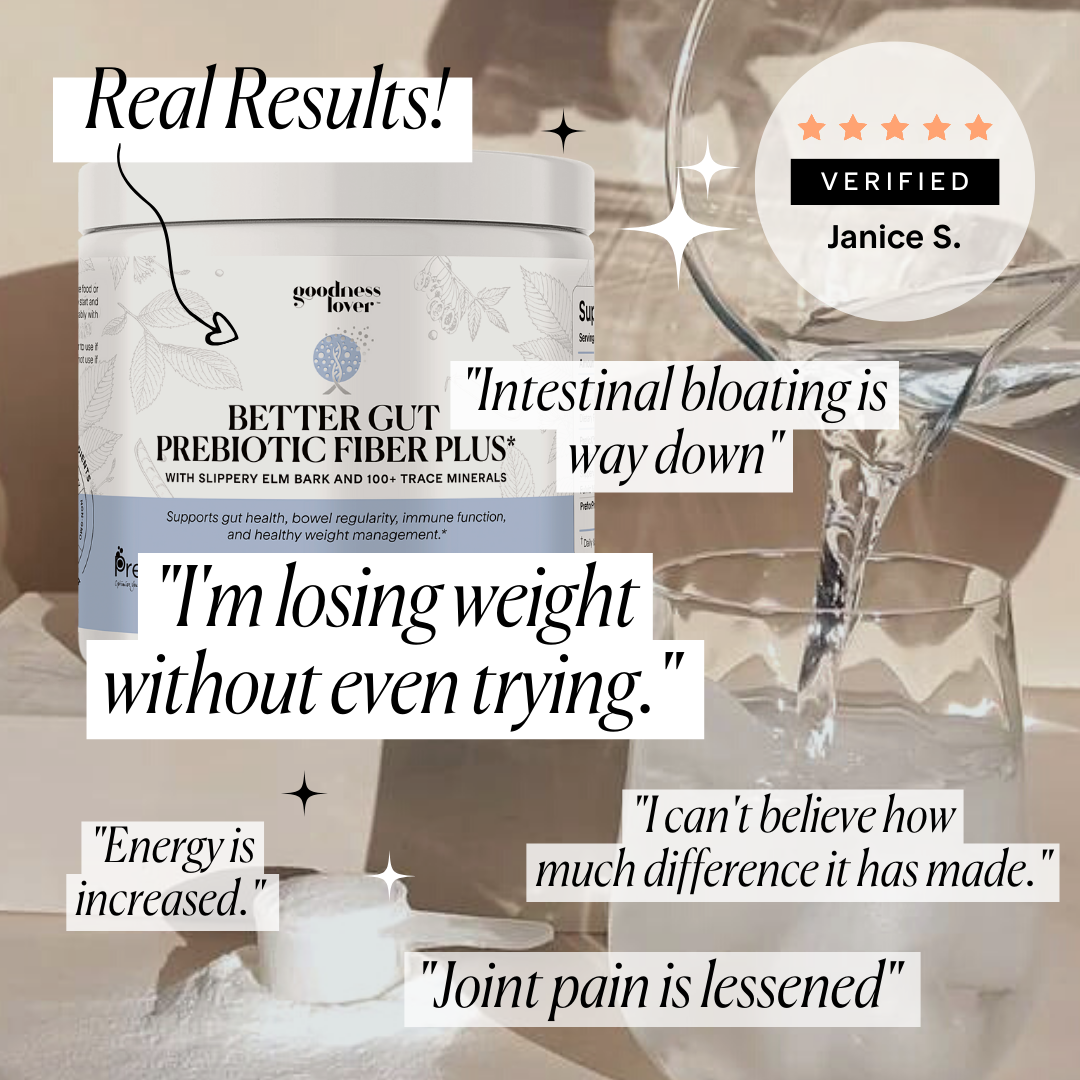
After figuring out and removing the drivers, add some gut-healing foods such as green smoothies and pre- and probiotic foods. Probiotics are various forms of good bacteria which are necessary to rebalance the gut ecosystem by overpowering the bad bugs by increasing the good ones. Some food sources include sauerkraut, kimchi, kombucha, kefir and coconut yogurt with live bacteria. It’s also ideal to obtain probiotics from a mix of food and supplement forms. Make sure you buy high strength and high-quality probiotics with a variety of different strains. Prebiotics are types of fiber that feed the good bacteria in your gut. There are many fruits and vegetables that are high in prebiotics as well as legumes, nuts and certain grains. Be careful though if you are sensitive to FODMAP as many foods that are high in prebiotics are also high in FODMAPs
3. Supplement with nutrients to restore healthy gut function
There are various herbal remedies and nutritional supplements that aid in restoring healthy gut function, reducing inflammation as well as in reducing symptoms. Nutrients such as zinc and magnesium are essential for the production of stomach acid to be able to break down your food properly as well as for the immune system, detoxification and stress management. Digestive bitters or enzymes help to ensure your food is fully digested as poorly digested food particles and proteins damage the intestinal wall. Nutrients such as L-glutamine, quercetin, vitamin A, vitamin D and zinc are essential for rebuilding the integrity of your gut wall and herbal remedies such as aloe vera, deglycyrrhizinated licorice, slippery elm and curcumin are also beneficial in reducing inflammation, restoring the mucosal lining of the gut and relieving digestive symptoms such as bloating and constipation.
4. Mitigate stress with some key stress management strategies
Chronically elevated stress hormones impact your digestion by reducing digestive enzyme function, disrupting GIT motility and causing dysbiosis. Getting enough sleep, exercising, getting out in nature and practicing gratitude are some great ways to alleviate stress. Supplements such as magnesium, Rhodiola, Withania, Licorice and Siberian Ginseng can also help to balance your adrenal glands, the ones responsible for producing your stress hormones.











What Do You Think? Comment Below: