Chronic pain and inflammation ruins lives. Simple things many of us take for granted, such as brushing our hair or getting out of bed in the morning can become painful activities. These symptoms not only affect you physically but emotionally as well and can have injurious effects on your relationships with your family and friends.
But did you know that inflammation largely stems from your gut? Your microbiome and the integrity of your gut wall help to keep inflammation at bay. If your gut wall is compromised and becomes “leaky,” harmful things can enter your bloodstream and incite an immune response which can lead to body-wide inflammation.
Tune in to this video to hear experts share about what causes inflammation in the gut so you can reduce pain and inflammation in your body and improve your quality of life.
Transcript: The Surprising Truth About Inflammation and the Gut
Sarah:
February 23, 2004. On the front cover of Time magazine, there is a fiery silhouette with the words “The Secret Killer.” Who was this secret killer? Or more precisely, what was this secret killer?
As scientists across the world delved deeper into the fundamental cause of disease, they were starting to see a common thread between them all. The silent killer was not some superbug or a genetic mutation or a chemical in our food. These scientists found one thing that lies at the core of all disease, and that one thing is actually one of our major immunological defense mechanisms. The silent killer is inflammation.
Dr. Nirala Jacobi:
Interestingly enough, when you get sick, the symptoms of being sick is actually not the pathogen or the virus or the invader, it's actually your own immune system being mobilized. And it speaks to, these two different branches, speak to one another through chemical messengers called cytokines. Cytokines tell the body to increase inflammation or decrease inflammation and to mobilize or to not mobilize. So, this is the chemical network that helps to mobilize either immune branch or immune system branch.
Sarah:
As you can see, inflammation is actually a normal response to an injury or infection. When your body is under threat, the immune system mounts an inflammatory response to help neutralise the threat and restore function. An inflammatory messenger increases blood flow to the injured area, bringing additional nutrients and white blood cells to kick-start the healing process.
However, sometimes our inflammatory immune response doesn’t shut down. And this is when inflammation becomes a problem. If this inflammatory response does not resolve the threat, your immune system gets stuck to the “on” setting, releasing harmful chemicals that can damage cells, affect organ function, and can eventually lead to a dysregulated immune system and chronic disease.
So what triggers this inflammatory process to go wrong in the first place?
Dr. Maura Henninger:
Inflammation in the gut is driven by a couple of things. One, something called leaky gut, second dysbiosis, or an imbalance of your bacteria in the gut. So both of those things can cause inflammation and inflammation typically the mechanism that results in is called the release of LPS or lipopolysaccharides.
Dr. Peter Bongiorno:
The microbiome impacts the immune system in a very profound way.
What the bacteria put out in terms of molecules and chemicals and things that they produce metabolically are going to greatly impact whether the immune system is a healthy immune system, whether it's an overactive immune system or whether it's an underactive immune system. Depending on the strains of the bacteria, all the different ones that are out there, they're also going to play a role.
There are some bacteria that are more pro-inflammatory. There are some bacteria that are more anti-inflammatory and even more, sometimes it's just the balance between the two that are going to help decide how inflamed the immune system might be.
Dr. Will Cole:
So to really understand inflammation, which is a product of the immune system to deal with autoimmune issues, these immune-mediated issues, you have to look at where the predominance of the immune system resides, which is in the gastrointestinal system. So things like candida overgrowth, things like SIBO are both linked to inflammatory and autoimmune problems.
Sarah:
It’s simple. How healthy our gut is matters when it comes to inflammation. Our diet, lifestyle and environment determine its biodiversity and resilience. So if you’re consuming the Standard American Diet (in other words, the SAD diet), which is high in saturated fat, salt, and refined carbohydrates and sugars, this is going to be feeding the pro-inflammatory bacteria in your gut, and essentially starving the bacteria that are good for you. If you’re drinking a lot of alcohol, taking antibiotics, not getting adequate sleep, and not exercising, this can also influence your microbiome, resulting in dysbiosis.
This dysbiosis blunts your immune response, triggers chronic inflammation, and can lead to disease from heart disease, diabetes, and neurological disorders, to allergies, autoimmunity and even cancer.
Dr. Peter Bongiorno:
The microbiome influences our risk of long-term, chronic disease also quite significantly. For example, it's well known that women, when they're young and they take antibiotics, they tend to have a much higher risk of breast cancer later on in life. Now, why would that be? Well, what we're learning is it's because the antibiotics destroy the good bacteria in the gut, the microbiome, and when that gut bacteria is destroyed, a woman can't process estrogens the way she normally needs to, which results in excess estrogens in the bloodstream and in the body, which can help promote breast cancer risk.
Sarah:
And last but not least, stress is a major driving force behind inflammation due to its effect on the gut.
Dr. Carrie Jones:
Cortisol can really influence the function of the gut. Cortisol and its buddies, adrenaline, which is epinephrin and noradrenaline, which is norepinephrine. Can really cause a breakdown in our mucus layer. So in our intestines we have… It's a tube, right? It's a tube. And what protects the upper and lower and sidewalls is this layer of mucus that's the trap, nasty things that come through. We need this mucus layer. But over time, high stress, high levels of adrenaline, high levels of cortisol wear down the mucus layer. And now it could expose pieces, parts of your wall. And that leaves it more susceptible to attack, to infection, to things getting through that shouldn't get through. So the commonly used phrase is it can increase your risk for leaky gut.
Sarah:
So when these various compounds, and most often it is food proteins, seep through the gut lining, your immune defense system will fight like hell to get rid of them. It will start to create antibodies against these foods because it thinks they are foreign invaders. What were previously harmless foods, are now treated like the bad guys and greeted with an inflammatory immune response every time they enter the body and so you enter this state of always being inflamed. And this is how a leaky gut can cause chronic inflammation that manifests in a whole range of symptoms including bloating, constipation, fatigue, skin rashes, brain fog, depression, and anxiety.
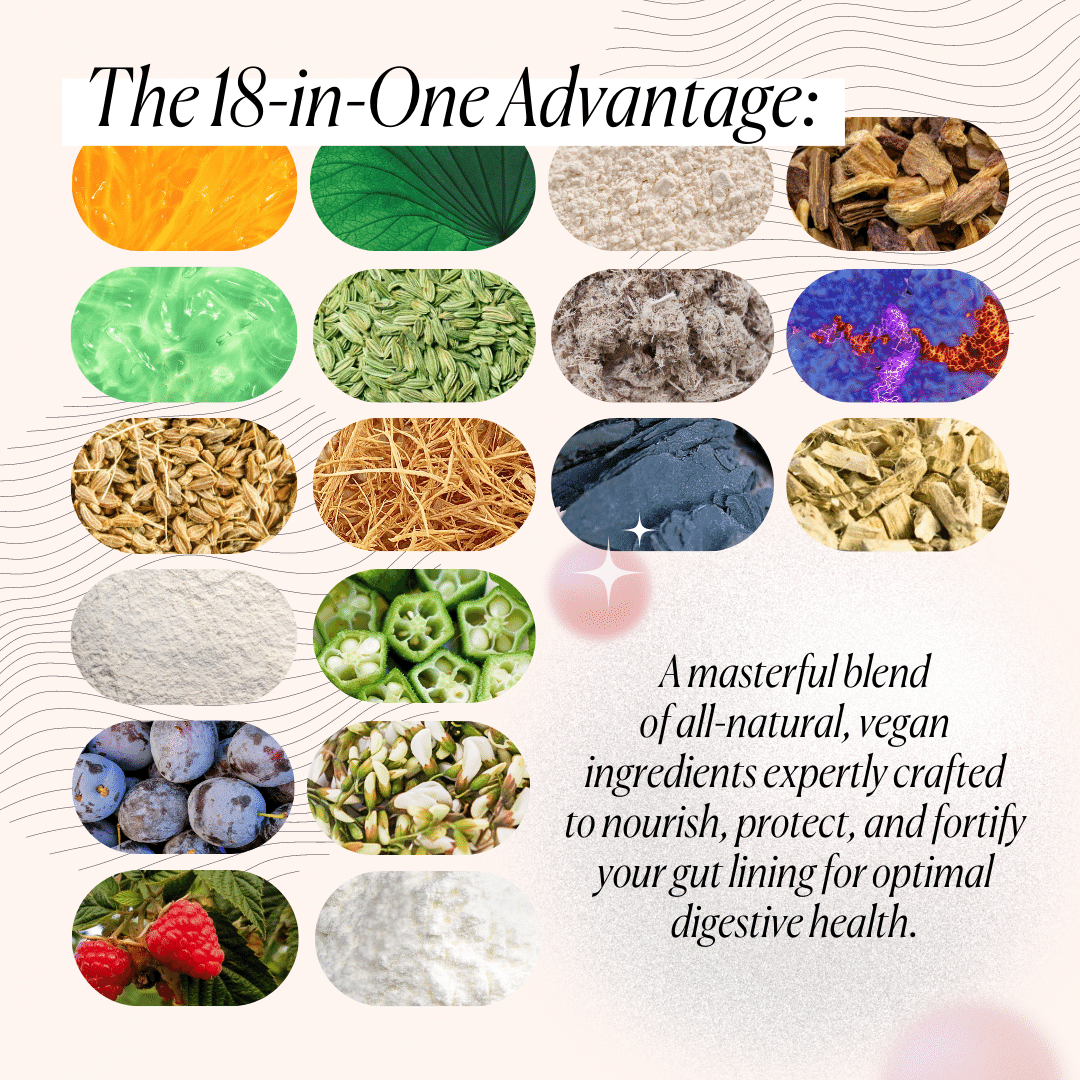
And therefore, the key to resolving inflammation, lies in healing your gut wall and restoring your microbiome.
Simply put, chronic pain and inflammation ruins lives.
Simple things many of us take for granted, such as brushing our hair or getting out of bed in the morning can even become painful activities. These symptoms not only affect you physically but emotionally as well and can have damaging effects on relationships with family and friends.
If inflammation is something you struggle with, we would love to hear from you. Please share with us in the comments how inflammation affects your life and please like and subscribe so more people can benefit from this information.
And if you want to learn more about how you can restore your microbiome and prevent inflammation, check out this video here where you can learn the top 5 ways to fortify your microbial defense system.








What Do You Think? Comment Below: