Have you ever felt like you're doing everything right for your hormones—eating well, managing stress, getting enough sleep—but you're still dealing with stubborn PMS, cyclical acne that won't quit, or periods so heavy they disrupt your life?
You're not imagining things. And you're definitely not alone.
Here's what most women don't know: there's a hidden player in your hormone balance that has nothing to do with your ovaries and everything to do with your gut. It's called the estrobolome—a specialized collection of bacteria living in your digestive system with one dedicated job: managing your estrogen levels.
Understanding your estrobolome might finally connect the dots between your gut symptoms and your hormonal chaos. And the best part? Once you know what's happening, you can actually do something about it.
Let's start with what this bacterial community actually is—and why it has so much power over your hormone balance.
Table Of Contents:
What Exactly Is the Estrobolome?
The estrobolome is a specific collection of gut bacteria that have one specialized job—metabolizing estrogen. These bacteria produce an enzyme called beta-glucuronidase. If that sounds technical, just think of it as molecular scissors. These scissors have the power to "cut open" packaged estrogen and release it back into circulation.
But first, a quick reminder about why this matters: estrogens are primarily made in the ovaries and adrenal glands. There are three different types, all of which play vital roles in the body. In women, estrogens help regulate body fat, are essential for reproductive function, cardiovascular health, bone health, and brain function (including memory). In men, estrogens aid in the maturation of sperm and maintenance of libido. So estrogen isn't just a "female hormone"—it's crucial for everyone.
In a healthy, balanced gut, you have low levels of this beta-glucuronidase enzyme. Your beneficial bacteria keep things in check, and estrogen flows out of your body smoothly.
But when your gut is in a state of dysbiosis—an imbalance where unhelpful bacteria outnumber the good ones—those beta-glucuronidase levels can skyrocket. Suddenly, you've got way too many scissors cutting open packages that were supposed to leave your body.
The consequences of elevated beta-glucuronidase levels extend far beyond uncomfortable symptoms. Research has linked high levels of this enzyme to serious health conditions including pre-menstrual syndrome (PMS), obesity, metabolic syndrome, estrogen-related cancers (breast and prostate), endometriosis, infertility, mood disturbances, and heart disease. This is why keeping this enzyme in check isn't just about feeling better—it's about protecting your long-term health.
The goal isn't to eliminate this enzyme completely. It actually serves a purpose in small amounts. The key is keeping its activity in a healthy, low range so your body can maintain hormonal balance.

How Your Body Should Handle Estrogen: The 2-Step Process
To understand what goes wrong, you need to know what right looks like. When your body is functioning beautifully, estrogen clearance happens in two clean steps.
Step 1: The Liver "Packages" Estrogen
Think of your liver as a processing plant. Once estrogen has done its job as a messenger in your body, it becomes "used" and needs to be deactivated. Your liver takes this circulating estrogen from your bloodstream and chemically changes it through a process called conjugation.
Imagine your liver neatly wrapping up the estrogen, putting it in a package, and marking it "ready for disposal." This packaged estrogen is then sent to your gut via bile, all set to leave your body for good.
Step 2: The Gut "Excretes" the Package
In an ideal world, that packaged estrogen travels through your digestive tract and exits your body with your stool. Simple. Clean. Done.
A healthy, balanced gut simply lets the package pass by without interference. The beneficial bacteria in your microbiome don't mess with it—they just let it move along toward the exit.
This is how it should work. Liver packages, gut excretes. Two steps, and your body maintains beautiful hormonal balance.
But here's the problem: this process often doesn't go as planned.
The Problem: When "Bad" Gut Bacteria Hijack the Process
When your gut is imbalanced, excess beta-glucuronidase cuts open the estrogen packages your liver worked hard to prepare. The "freed" estrogen—which was supposed to be deactivated and on its way out—gets reabsorbed through your gut lining and sent right back into your bloodstream.
It's a vicious cycle. Estrogen that was supposed to be eliminated is now back in circulation, adding to your body's total estrogen load. Your liver has to process it all over again, only for it to potentially get recycled again in your gut.
The Result: Estrogen Dominance
This recirculation is a major root cause of what's called estrogen dominance—when your estrogen levels are too high relative to your progesterone. This imbalance is behind so many of the hormonal symptoms that conventional medicine struggles to address.
Common symptoms of estrogen dominance include:
- Stubborn hormonal acne, especially along the jawline
- Worsening PMS—mood swings, anxiety, irritability
- Heavy, painful, or clotty periods
- Tender or fibrocystic breasts
- Cyclical headaches or migraines
- Unexplained weight gain, particularly around your hips and thighs
- Low libido
- Fatigue that gets worse with your cycle
This is why conventional approaches that focus only on hormones—without addressing gut health—often fall short. If your gut is recycling estrogen back into your system, you're fighting an uphill battle.
The good news? Once you understand this connection, you can actually do something about it.
Signs Your Estrobolome Might Need Support
So how do you know if your estrobolome is part of the problem? Here are the key signs that your gut bacteria might be interfering with healthy estrogen clearance.
Hormonal Red Flags
Watch for hormonal issues that started or worsened after antibiotic use, which can significantly disrupt your gut bacterial balance. PMS that's progressively getting worse over time, perimenopause symptoms that feel extreme or unmanageable, or hormonal patterns that just don't respond to conventional approaches all warrant attention.
The Gut-Hormone Overlap
One of the biggest clues is when digestive and hormonal symptoms show up together. Pay attention if you experience bloating that worsens with your menstrual cycle—this often indicates that hormonal fluctuations are affecting your gut, and vice versa.
Constipation is a major red flag for estrogen issues. If you're not having at least one complete bowel movement daily, estrogen that should be leaving your body is sitting in your digestive tract, giving beta-glucuronidase more time to reactivate it.
IBS symptoms that fluctuate with your hormonal changes, or any history of digestive issues alongside hormonal symptoms, suggest your gut and hormones are influencing each other.

Lifestyle & History Factors
Certain lifestyle patterns can compromise your estrobolome. Recent or frequent antibiotic use is one of the biggest disruptors of healthy gut bacteria. A diet low in plant fiber and diversity doesn't provide the food your beneficial bacteria need to thrive.
High intake of processed foods and sugar feeds the unhelpful bacteria that produce excess beta-glucuronidase. And chronic stress affects both your gut lining integrity and your hormone balance, creating a perfect storm for estrobolome dysfunction.
If several of these signs resonate with you, supporting your estrobolome could be the missing piece in your hormone balance puzzle.
How to Support Your Estrobolome Naturally
Now for the part you've been waiting for—what you can actually do about this. The good news is that supporting your estrobolome is entirely within your control, and the strategies are practical and accessible.
First, let's be clear about what we're aiming for. We're not trying to eliminate beta-glucuronidase entirely—it serves a purpose in small amounts. The goal is rebalancing your gut microbiome to keep enzyme activity in a healthy, low range while supporting both steps of the estrogen clearance process: liver packaging and gut elimination.
1. Nourish the Good Bacteria (Prebiotics)
Your beneficial bacteria need food to thrive, and that food is diverse plant fiber. These fibers feed the bacteria that maintain your gut lining integrity and keep your estrobolome balanced.
Try the 30-plant challenge: aim for 30+ different plant foods weekly. This isn't as hard as it sounds—herbs, spices, nuts, seeds, vegetables, fruits, legumes, and whole grains all count.
Focus on prebiotic-rich foods like flaxseeds, garlic, onions, asparagus, Jerusalem artichokes, and slightly green bananas. Add in polyphenol-rich foods like berries, green tea, dark chocolate, and colorful vegetables—these compounds feed beneficial bacteria and reduce inflammation.
Practical tip: each meal is an opportunity to add 2-3 different plant foods. Sprinkle seeds on your breakfast, add multiple vegetables to lunch, include herbs and spices in dinner.

2. Support Your Liver (Step 1 of the Process)
Your liver needs specific nutrients to package estrogen efficiently the first time. If this step isn't working well, you're already starting behind.
Cruciferous vegetables are absolute superstars here—broccoli, cauliflower, kale, Brussels sprouts, and cabbage contain compounds that support both liver detoxification pathways and healthy estrogen metabolism. They're rich in DIM (diindolylmethane), a natural compound that helps your body process estrogen into beneficial metabolites.
Here's an added bonus: cruciferous vegetables are also rich in glucaric acid, a natural compound that inhibits beta-glucuronidase activity. Research has found that oranges, apples, grapefruit, and cruciferous vegetables contain the highest concentrations of glucaric acid among common foods.
Aim for at least one serving of cruciferous vegetables daily. Other liver supporters include adequate protein (your liver needs amino acids for conjugation), B vitamins, magnesium, glutathione, and sulfur-rich foods like garlic and onions.
3. Optimize Estrogen Elimination Through the Gut
Even if your liver packages estrogen perfectly and your estrobolome is balanced, you still need to get that estrogen out of your body. This is where fiber becomes crucial again—it binds to estrogen in your digestive tract, preventing reabsorption.
Support elimination through soluble fiber (such as psyllium, glucomannan), adequate hydration, and regular movement—exercise supports gut motility and helps move things along.
4. Reduce Inflammatory Triggers & Estrobolome Disruptors
It's not just about what you add—it's also about what you remove. Minimize foods that feed unhelpful bacteria, particularly processed foods, excess sugar, and artificial sweeteners.
Be strategic with antibiotics—use them only when medically necessary, and restore your microbiome afterward with prebiotic support and plant diversity.
Reduce exposure to environmental estrogens (xenoestrogens) found in plastics, conventional personal care products, and pesticides. These compounds mimic estrogen in your body and add to your total estrogen load.
Moderate alcohol intake—alcohol affects both your estrogen levels and your gut bacterial balance. And prioritize stress management, because chronic stress damages your gut lining and disrupts both your microbiome and hormone balance.
5. Assess & Heal the Gut with Functional Testing
If you want to take the guesswork out of the equation, comprehensive stool analysis can be incredibly valuable. This testing can identify dysbiosis, actually measure your beta-glucuronidase levels, and assess your beneficial bacteria populations.
A personalized approach based on testing reveals your specific imbalances rather than having you guess. You can then create targeted healing protocols that address your unique findings—whether that's low beneficial bacteria, high pathogenic bacteria, or gut inflammation.
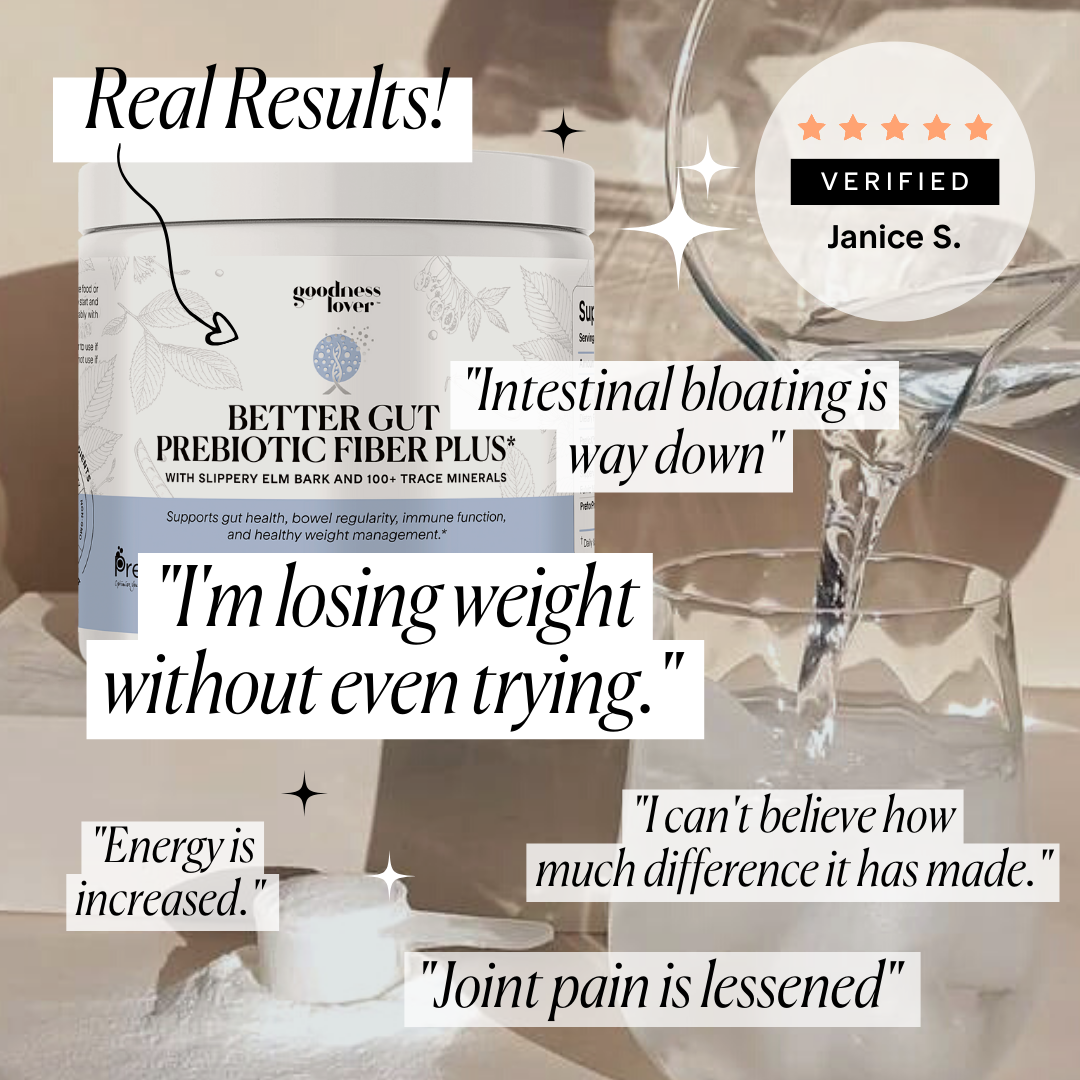
6. Consider Targeted Supplementation
While food should always be your foundation, certain supplements can provide additional support.
Calcium-D-Glucarate: This is one of the most well-studied natural beta-glucuronidase inhibitors. Studies show that calcium-D-glucarate supplementation can inhibit beta-glucuronidase activity in serum and intestinal tissue by 39-70%, depending on the dose and location. Research has demonstrated its effectiveness in supporting healthy estrogen elimination and has even been studied for its role in cancer prevention.
Specific Probiotic Strains: Not all probiotics are created equal when it comes to estrogen balance. Research has identified specific strains that reduce beta-glucuronidase activity:
- Lactobacillus rhamnosus GG and Lactobacillus acidophilus have been shown in animal studies to significantly decrease beta-glucuronidase activity in the gut
- Bifidobacterium breve and Lactobacillus casei Shirota contribute to changes in intestinal microbiota that lower beta-glucuronidase activity
- Bifidobacterium longum has demonstrated the ability to reduce this enzyme activity in clinical trials
Prebiotic Fiber Supplements: When dietary intake needs additional support, prebiotic supplements containing oligofructose-enriched inulin have been shown in research to reduce beta-glucuronidase activity. These prebiotics feed the beneficial bacteria that help maintain healthy estrobolome function.
Important note: always consult with a healthcare provider before starting supplements, especially for hormone-related concerns. What works for one person may not be appropriate for another, and professional guidance ensures you're taking the right approach for your body.
Your Gut Is Your Hormones' Partner
Here's the paradigm shift: your hormonal health is directly tied to the health of your gut. They're inseparable partners.
Your gut bacteria are active participants in hormone regulation—not passive bystanders. The estrobolome can be either your greatest ally or your hidden obstacle.
Start with one change today: increase your fiber diversity, add daily cruciferous vegetables, or reduce one gut disruptor. Focus on supporting both liver packaging and gut elimination.
Hormone balance isn't a mystery—for many, it's a gut issue with real solutions.










What Do You Think? Comment Below: