Picture this: you're a brave knight, clad in shining armor, wielding a powerful sword to vanquish the evil dragon that has been terrorizing your kingdom. In this epic battle, your sword represents antibiotics, the dragon symbolizes harmful bacteria, and your kingdom is none other than your body.
But wait, there's a twist! Unbeknownst to you, your kingdom is also home to a thriving community of friendly dragons (yes, they exist!) that help maintain peace and prosperity. These good dragons represent the microbiome, and they, too, are affected by your mighty sword.
Antibiotics, our metaphorical sword, have been a game-changer in modern medicine. Since their discovery, they have saved countless lives by effectively combating bacterial infections. However, as with any powerful weapon, wielding antibiotics comes with great responsibility. While they are incredibly effective at slaying the bad bacteria, they can also inadvertently harm the bustling metropolis of beneficial microorganisms that call our bodies home.
These microscopic inhabitants play a crucial role in our overall health, from digestion and metabolism to immune system support and even mental health. Alas, the indiscriminate nature of antibiotics can disrupt this delicate balance, leading to a cascade of consequences that we are only just beginning to understand.
So, join us as we delve into the complex relationship between antibiotics and the microbiome, exploring the good, the bad, and the downright microscopic. Together, we'll learn how to wield our antibiotic swords responsibly, ensuring the safety of our friendly dragons and the prosperity of our kingdoms.
Table of Contents:
What Are Antibiotics?
The term "antibiotics" refers to a class of drugs that are used to treat bacterial infections by either killing bacteria or inhibiting their growth.
The story of antibiotics began in 1928 when Sir Alexander Fleming, a Scottish bacteriologist, stumbled upon the mold Penicillium notatum. This unassuming mold turned out to be a game-changer, as it produced a substance capable of killing a wide range of bacteria. This substance, later dubbed penicillin, marked the dawn of the antibiotic era. Since then, numerous other antibiotics have been discovered and developed, each brandishing their own unique bacteria-busting abilities.
Antibiotics come in various shapes and sizes, or more accurately, different chemical structures, spectrums of activity, and modes of action. Some common classes include penicillins, cephalosporins, tetracyclines, and macrolides. These different classes of antibiotics target specific bacterial processes, such as cell wall synthesis, protein synthesis, or DNA replication, ultimately leading to the demise of the harmful bacteria.
Do Antibiotics Live Up To The Hype?
- Antibiotics disrupt microbiome balance
Unfortunately, antibiotics don’t only target the evil dragons (bad bacteria), they also inadvertently wipe out some of our friendly dragons in the process.
These friendly microbial dragons play a crucial role in maintaining the balance within our microbiome, and their loss can create a void that allows harmful bacteria to thrive. For example, the use of certain antibiotics can lead to the overgrowth of the notorious Clostridium difficile, a bacterium responsible for severe diarrhea and colitis. This opportunistic pathogen takes advantage of the disrupted microbiome and establishes itself as an unwelcome guest in our gut.
- Short-term effects of antibiotics on the microbiome
Antibiotics can also knock you sideways with some nasty side effects.
One common short-term effect of antibiotic use is gastrointestinal issues, such as diarrhea, nausea, and abdominal pain. Antibiotic-associated diarrhea (AAD) affects up to 30% of patients taking antibiotics, with the severity ranging from mild to severe.
This occurs because antibiotics can disrupt the balance of our gut microbiota, leading to a decrease in beneficial bacteria that help maintain gut health. In some cases, this can even result in a more severe form of diarrhea caused by the overgrowth of Clostridium difficile, as we mentioned earlier.
By disrupting our gut ecosystem, antibiotics also leave us vulnerable to opportunistic pathogens.
This can lead to an elevated risk of developing infections, particularly those caused by antibiotic-resistant bacteria.
- Long-term effects
The disruption of our microbial communities can have lasting effects on our health.
In fact, studies reveal that changes in our gut bacteria could be behind a range of chronic ailments like obesity, type 2 diabetes and inflammatory bowel disease. Our gut bacteria may trigger chronic inflammation and disrupt our body's metabolic machinery, paving the way for these diseases.
Also, not only does a disrupted microbiome leave us more vulnerable to fend off infections, it can leave us more susceptible to autoimmune and allergic diseases. Finally, disruptions in the gut microbiota have been linked to human brain diseases such as anxiety, depression, and even neurodevelopmental disorders like autism. 
- Antibiotics are over-prescribed, creating “superbugs”
Undoubtedly, antibiotics are life-saving and have literally saved millions from deadly diseases.
But, despite their glory, the reality is, they are being overprescribed like crazy. Many healthcare professionals prescribe antibiotics without double-checking if they will actually effectively attack the bug, or even confirming if it's a bacteria or a virus, against which antibiotics are completely ineffective.
In fact, the Center for Disease Control and Prevention has estimated that a whopping four out of five Americans are given antibiotics every year for ailments that don't even require them. This has led to the rise of antibiotic-resistant “superbugs.”
The term "superbugs" refers to bacteria that have developed resistance to multiple antibiotics, making them incredibly difficult to treat. According to a report by the World Health Organization, “Antibiotic resistance is one of the biggest threats to global health, food security, and development today,” with an increasing number of bacterial infections, such as pneumonia, tuberculosis, and gonorrhea, becoming harder to treat.
The primary driver behind this alarming trend is the overuse of antibiotics, both in human medicine and agriculture. When antibiotics are used excessively or inappropriately, it creates an environment where only the strongest, most resistant bacteria survive and multiply. As these superbugs continue to evolve and spread, we risk returning to a pre-antibiotic era, where even minor infections could prove fatal.
What You Can Do To Minimize The Impact Of Antibiotics
This all sounds like the plot of a dystopian sci-fi novel, right? Unfortunately, this scenario is all too real, thanks to the rise of these antibiotic-resistant "superbugs."
So, where does that leave us?
Well, it definitely highlights the importance of adopting a more judicious approach to antibiotic use and emphasizes the need for implementing strategies to minimize their impact on our gut health.
1. Responsible antibiotic use
First and foremost, responsible antibiotic use is key. This means taking antibiotics only when they are absolutely necessary (in less than 20% of the infections seen in primary care). By using antibiotics judiciously, we can help preserve the delicate balance of our microbiome and reduce the risk of antibiotic resistance. Additionally, it's essential to complete the full course of antibiotics as prescribed, even if you start feeling better before finishing the medication. This ensures that the infection is fully treated and reduces the risk of relapse or resistance.
2. Using natural alternatives to antibiotics
What many people don’t know is that nature offers us a plethora of natural antibiotics that have antibacterial and antiviral properties to fight infection. Some examples include reishi and shiitake mushrooms which contain antibiotic components that inhibit gram-positive and gram-negative bacteria. In fact, research has found shiitakes to be effective against 85% of pathogens that it has been tested on, including many species of mold and yeast!
Echinacea, elderberry, olive leaf extract, and golden seal are some herbal remedies that have a long history of use as antimicrobials and antivirals in traditional medicine. Echinacea for example, is effective for use against numerous infections including gum disease, herpes, malaria, syphilis, typhoid, UTIs, and yeast infections. Zinc and vitamin C are also some great nutrients to add to the mix due to their involvement in immune function. 
3. Take probiotics and prebiotics
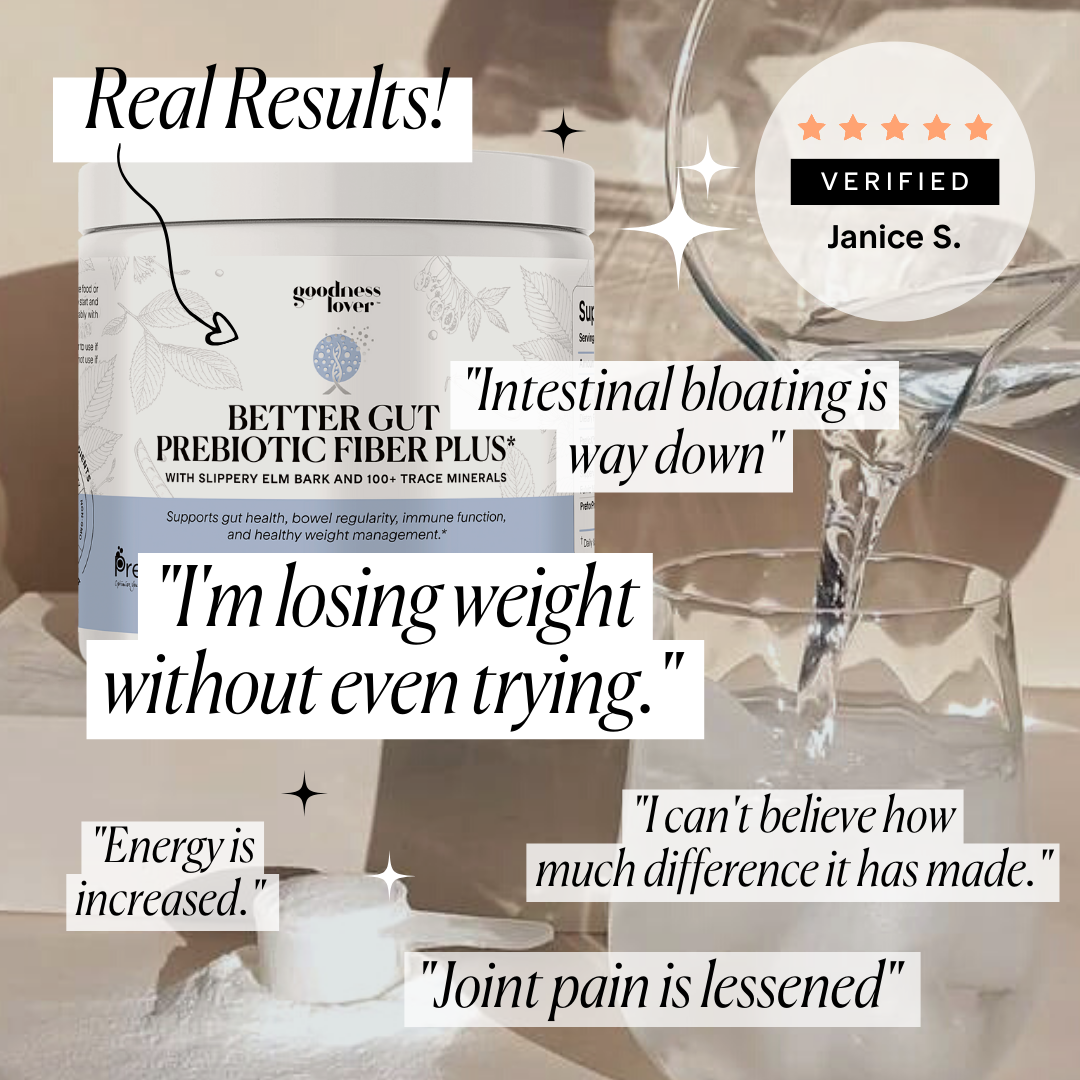
After completing a course of antibiotics, it's essential to focus on restoring the balance of your gut microbiome, and this is where probiotics and prebiotics come into play. Probiotics are live microorganisms that can help replenish the beneficial bacteria in your gut, while prebiotics are non-digestible food components that promote the growth and activity of these friendly microbes. By incorporating both probiotics and prebiotics into your diet, you can support the recovery of your gut microbiota and maintain a healthy balance of bacteria.
Some of the best probiotic strains to consider after antibiotic use include Lactobacillus rhamnosus GG, Saccharomyces boulardii, Lactobacillus acidophilus NCFM, and Bifidobacterium lactis Bi-07. To maximize the benefits, pair these probiotics with prebiotic-rich foods, such as whole grains, bananas, onions, and garlic, as well as probiotic-rich foods such as yogurt, kefir, sauerkraut, and kimchi, to nourish and support the growth of your gut's beneficial bacteria.
4. Lifestyle changes
Lastly, don't underestimate the power of a healthy lifestyle in supporting your microbiome. A balanced diet rich in fruits, vegetables, and whole grains can provide the necessary nutrients and fiber to nourish your gut bacteria and reinforce your defence systems. Regular exercise has also been shown to positively influence the composition and diversity of the gut microbiome, contributing to overall health. Additionally, managing stress through practices such as mindfulness, meditation, or yoga can help maintain a healthy gut-brain axis and support both your mental and physical well-being.
Final Thoughts
So, the next time you find yourself reaching for that antibiotic prescription, remember the trillions of microscopic allies that call your body home and consider the impact on their delicate ecosystem.
By practicing responsible antibiotic use or using natural alternatives, nourishing your gut with probiotics and prebiotics, and embracing a healthy lifestyle, you can help maintain a harmonious relationship with your tiny, yet mighty, microbial friends.
After all, a healthy, harmonious microbiome is a happy microbiome, and who wouldn't want to keep their invisible sidekicks (fighting dragons) in tip-top shape?
Recipe Spotlight: Baked Giant Lima Beans in Tomato Sauce
This is a delicious and hearty Mediterranean dish to be enjoyed with a salad or bread. These giant white beans are buttery and tender. They are first boiled, then cooked in the oven with herbs and spices. Lima beans are a great source of protein as well as being low GI. They’re also packed with fiber to feed those good bugs in our gut, help regulate blood sugar and boost our immune system. Enjoy!













What Do You Think? Comment Below: