If you were paying attention at all in your high school biology class, then you’ll likely remember hearing about your mitochondria.
You would certainly remember mitochondria to be the powerhouse of your cells, but what exactly do they do? How are they related to the health of our gut? And what can we do to support the health and function of our mitochondria?
Table Of Contents:
What are mitochondria?
Your mitochondria are the tiny cellular components responsible for generating adenosine triphosphate (ATP), the energy that keeps you and your cells alive.
The body relies on an incredible number of mitochondria to fuel its cells. Especially for neurons, retinal cells in the eye, heart muscle and liver hepatocytes - these high-energy demanding cell types contain thousands upon thousands of vital organelles that help keep you healthy!
Your mitochondria are essentially the battery (or powerhouse) of each of the cells in your body. They take the oxygen you breathe and use it to make more than 95% of your body’s energy!
Mitochondria not only provide energy to cells, they are also involved in a host of other function. By regulating certain key signalling molecules such as calcium and reactive oxygen species (ROS), these powerhouses have their fingers in many pies- setting off a chain reaction that affects inflammation, cell death processes, innate immunity, and autophagy.
They help create vital hormones and regulate vitamin D. Acting as tiny chemical factories within organs like the adrenals, gonads, placenta and brain, their role is even further extended to modulating calcium levels needed for proper hormonal signaling.
When our mitochondria don't hum along at optimal capacity, the functions of every cell in the body suffers - and so does our health. To achieve peak performance of both mind and body you must prioritize mitochondrial wellbeing, for no other effort can make up for what these strong energy-producing cells provide!
Mitochondria in health and disease
While the scientific community has long been aware of the importance of mitochondrial function in maintaining health, it is only recently that its significance is becoming more widely recognized. When functioning correctly, we can live life feeling energized - however if mitochondrial dysfunction occurs, our health can suffer in many ways.
In the past years, mitochondria have been identified as significant players in the ageing process. As a result, they are being studied for their role in the development of age-related chronic conditions such as cancer, neurodegenerative disorders, heart disease, and age-related muscle decline.
A slew of factors are believed to fuel mitochondrial-driven aging and disease, including impaired enzyme activity, increased production of ROS, depletion of antioxidant reserves, mutations in the mitochondria's DNA and an accumulation of damaged mitochondria, and misfiring electron transport chains.
Mitochondrial dysfunction has been linked to a wide variety of conditions, including, but not limited to:
-
Autoimmune conditions, such as systemic lupus erythematosus, and multiple sclerosis
-
Neurodegenerative disorders, such as Alzheimer's disease and Parkinson's
-
Psychiatric conditions such as bipolar disorder, depression, schizophrenia
 Mitochondria play an important role in neurologic health and mental health. If you’re experiencing mitochondrial dysfunction, you won’t be able to produce enough energy to fuel other enzymatic processes such as serotonin and dopamine production, neurotransmitters that are essential for mental health. This means you are likely to feel anxious or depressed, tired, and unmotivated.
Mitochondria play an important role in neurologic health and mental health. If you’re experiencing mitochondrial dysfunction, you won’t be able to produce enough energy to fuel other enzymatic processes such as serotonin and dopamine production, neurotransmitters that are essential for mental health. This means you are likely to feel anxious or depressed, tired, and unmotivated.
Some other signs that your mitochondria are not working efficiently include an increase in fatigue, premature ageing, constant fatigue, chronic pain, feeling sick all the time, weight gain. Food cravings, difficulty focusing, forgetfulness, muscle weakness, exhaustion after mental pr physical exhaustion, and hormonal imbalances. Due to the vital role of ATP production, even a mild decrease in mitochondrial dysfunction may lead to symptoms.
What causes mitochondrial dysfunction?
As we get older, our mitochondria become gradually less efficient. However, there are certain lifestyle choices that can have a disastrous effect on their vitality - leaving us feeling exhausted and unwell at an earlier age than necessary.
1. Nutrition
Our mitochondria need an array of essential nutrients to produce energy, but when we don't fuel them properly, they start to malfunction. Eating a diet that is high in processed foods with little nutritional value and a lack of antioxidants, omega-3 fatty acids, vitamins, and minerals not only fails to provide what's needed for optimal mitochondrial functioning - but it can also even damage these vital organelles!
Some foods that are especially harmful to mitochondrial health include:
- Sugar
Eating too much sugar is a sure-fire way to cause harm to your body. An excessive intake of this sweet substance can quickly lead to dangerous insulin levels that spark an inflammatory response inside the body and even damage to your mitochondria.
Vegetable oils loaded with omega-6 polyunsaturated fatty acids, such as soybean oil, corn oil and sunflower oil can prove to be a perilous combination - their breakdown products can wreak havoc on our mitochondrial DNA.
-
Monosodium glutamate (MSG)
Monosodium glutamate has been found to decrease the efficiency of the body's antioxidant systems, ultimately resulting in weakened mitochondrial activity.
2. Environmental toxin exposure
In the modern world, our bodies are constantly exposed to dangerous toxins through the water and food we ingest and the air that fills our lungs. These hazardous materials can trigger an increase in free radicals known as reactive oxygen species (ROS). Unfortunately, mitochondria seem unable to resist the harmful effects that these free radicals can cause.
Alcohol consumption, in particular, can lead to mitochondrial dysfunction. We may enjoy the occasional drink, but continued alcohol consumption can lead to serious consequences. Our body's ability to combat oxidative stress caused by ethanol decreases with age and frequent imbibing - leaving our mitochondrial DNA vulnerable to damage.
Some other deleterious toxins to our mitochondria include glyphosate (the herbicide Roundup) and methyl-mercury.
3. Hormonal imbalances
The thyroid is a key player in energy production, releasing hormones that regulate mitochondrial activity. T3 is one such hormone as it prompts ATP production as well as growth in the number of mitochondria. If we have an underfunctioning thyroid or if there's an issue with the release or conversion of these hormones from our thyroids, it affects the function of our mitochondria.
Chronic fluctuations in another hormone, insulin, can also lead to mitochondrial dysfunction. Consuming too many carbohydrates on a regular basis can lead to higher-than-normal blood sugar levels, prompting the body's need for additional insulin production. As a result, the mitochondria responds to the body’s demand for energy by burning sugar instead of fat, though sugar is a less efficient source of fuel.
4. Dehydration
Water is essential for our bodies to properly function and generate energy. Not having enough of it can lead to a decrease in ATP production, making it even more difficult to hydrate the cells within us. Furthermore, simply drinking water isn't always enough - we must also have sufficient mitochondrial activity that creates a gradient necessary for the absorption of water into the cells in order to be utilized.
5. Viral infections
In a never-ending search for suitable hosts, viruses can cause immense harm to our cells. From the Epstein-Barr virus causing mitochondrial damage and increasing cancer risk to Herpes simplex type 1 (HSV1) disrupting calcium homeostasis and resulting in mitochondrial dysfunction within our nerve cells - some of these unwelcome guests establish permanent residence within us, leading to chronically damaging effects on our mitochondria.
6. Stress
Stress can have a profoundly negative effect on mitochondrial health, even indirectly. Elevated cortisol levels caused by stress can lead to poor fat metabolism and increased cravings for sugar - increasing the likelihood of viral infection. Additionally, our stressful lives often lead us down unhealthy paths such as eating high sugar, nutrient-deficient diets, or skipping out on adequate rest which further contributes to inhibited mitochondrial functioning.
Diagnosing mitochondrial dysfunction
There’s no guaranteed way to diagnose mitochondrial dysfunction but individuals with inherited mitochondrial disease may benefit from DNA testing or a muscle biopsy. If toxic exposure is suspected as causality for general mitochondrial dysfunction then an array of blood tests could provide answers and lead you towards the right diagnosis.
-
Lactic acid
-
Pyruvate
-
Carnitine (free and total) and an acylcarnitine panel
-
Ubiquinone
-
Ammonia
-
Urinalysis (ketosis without being on a ketogenic diet)
-
Creatine kinase
-
An AST/ALT ratio greater than 2
Your mitochondria and your microbiome
Your microbiome and your mitochondria have a direct line of communication with each other. Your mitochondria work together to not only regulate the diversity of bacteria within your gut microbiome but also create a unique environment that allows them to thrive. However, this relationship isn't always smooth-sailing; increased reactive oxygen produced by mitochondria can sometimes cause disruption within the microbial community of your gut.
On the other hand, new research shows that drastic shifts in our cellular and organ functions, energy production, and even mitochondrial DNA sequences can be traced back to a single source: the microbiome. The microbiome plays a significant role in the synthesis of chemicals such as bile acids, pyrroloquinoline, quinone, and fermentation gases that can shift mitochondrial function. If your microbiome is out of balance, you won’t be absorbing the nutrients that you need for mitochondrial ATP production.
Recent research has also uncovered that gut bacteria produce crucial metabolites such as short-chain fatty acids which affect mitochondria activity. These compounds are responsible for regulating inflammation levels as well as creating new mitochondria or ROS production - representing its immense importance within the body's inner workings.
Where to go from here?
Despite our best efforts to lead healthy lives, everyday can be full of hazards for our mitochondria. From stress and poor nutrition to environmental toxins, these threats compound in a relentless cycle that can lead to chronic inflammation, dysregulated blood sugar, and underperforming mitochondria.
All of this information can feel disheartening!
However, every day offers you a chance to improve your overall health and wellbeing by treating your mitochondria well. So, if you’re interested in increasing your health span, reducing your risk of disease, and improving your quality of life, you will no doubt want to know more about how you can support your mitochondrial health. So stay tuned for our article next week on how you can support your mitochondria naturally.
Recipe Spotlight: Roasted Tomato and Fennel Soup with Basil and Garlic Pesto
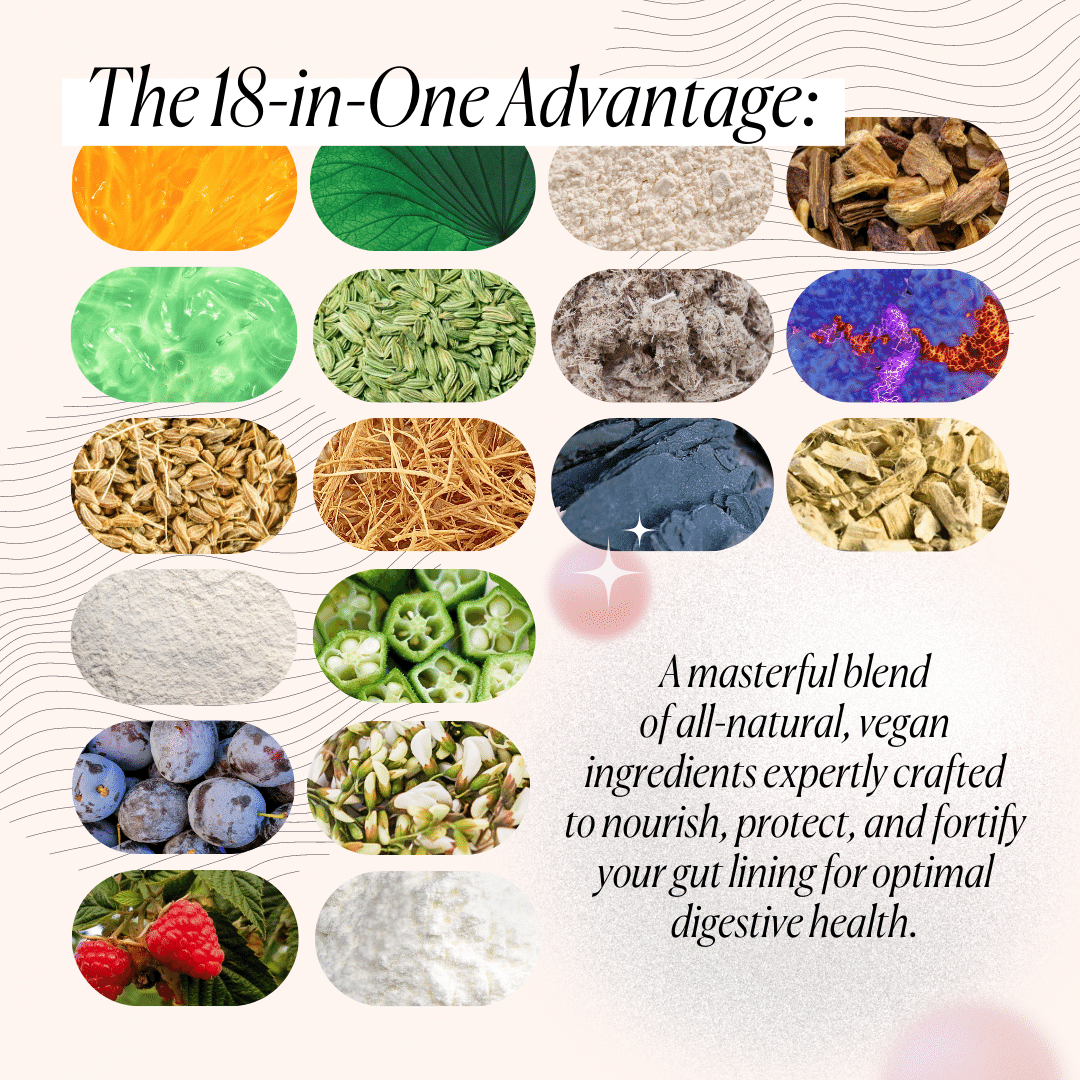
Nutrition is one of the biggest causes of mitochondrial dysfunction. Without essential nutrients, it will not be able to produce the energy that your body sorely needs.
So with our recipe, you’ll get a soup packed with vitamins and minerals that your mitochondria needs to function in top form. Best of all, we’ve added ingredients that will intensify its flavor, elevating what would otherwise be your run-of-the-mill tomato soup. Enjoy!












What Do You Think? Comment Below: