2000 years ago, the ancient physicians were onto something.
What formed the basis of their theories on health and disease was the concept that there is this connection between your mind and your body and that the treatment of one involves the treatment of the other.
A lot of evidence has emerged in the last few decades to confirm just how much the gut and the mind are inextricably linked. This bi-directional relationship or communication network between the gut and the brain has been coined the gut-brain axis. Much scientific research is accumulating that demonstrates just how fundamental a role it plays in maintaining digestive and mental health.
The Gut-Brain Axis
The gut-brain axis comprises several systems within the body, including the autonomic and enteric nervous systems, the central nervous system, and the hypothalamic-pituitary-adrenal (HPA) axis.
Neural, endocrine, immune, and humoral pathways are utilized to signal messages from the gut-microbiota to the brain and from the brain to the gut-microbiota. Research into the gut-brain crosstalk has revealed a complex communication network that not only ensures proper gastrointestinal homeostasis but also influences emotional and higher cognitive functions.
What the gut-brain axis means is that an imbalanced gut ecosystem and a weak intestinal barrier (a.k.a. leaky gut) can affect our nervous system, and vice versa—that our behaviors, thoughts, and feelings have the ability to influence the health of our gut, leading to poor health outcomes.
In short, your inner world can have a dramatic effect on your physical health.
What Stress Does To Your Body
So let’s take a look at this second scenario. How does stress impact our body?
Due to this connection between the gut and the brain, stress, in all its forms, can have a profound impact on our overall health.
Now stress is more than just those feelings that make the heart race and our brain frazzled. Stress can also be environmental (such as toxicity in the water that we drink or pollution in the air that we breathe), biological (such as an inflammatory diet or a nutrient deficiency), or even physical (like a stubbed toe). Childhood trauma is another common source of stress which can have ongoing debilitating effects.
Regardless of the stressor, our body produces stress hormones just in case that stressor poses a real physical threat to our life. Fortunately for us, the HPA axis is our very own in-built hormonal messaging system that helps to switch on the “fight or flight” response throughout the whole body.
The HPA axis is made up of our hypothalamus (the inbox of the brain or the part of our brain that receives stimuli), the pituitary gland (the hormonal messenger), and the adrenal gland (which is responsible for releasing our stress hormones such as cortisol).
When you’re facing a stressor of any kind—whether it’s being chased by a lion or an outstanding bill—your adrenal glands secrete cortisol and your body shifts into the sympathetic nervous system state. In this state, under the direction of signals from the brain, the body frees up stored sugars for a burst of energy, your heart rate and blood pressure increase, and your digestive system is temporarily put on hold. All this is done to give you the energy you need to escape from a risky situation or to stay and fight.
Now normally, once the stress has passed, hormones are released that trigger a shift back to the parasympathetic nervous system (which is the mode that supports digestion, healing, immunity, and proper metabolic function).
Unfortunately, often our stress today doesn’t go away, and our nervous system becomes stuck in this state of alarm.
When Stress Doesn’t Go Away
When we’re in this “fight or flight” alarm mode, we have higher levels of glucose circulating in our bloodstream. This, of course, prompts our pancreas to release more insulin to try and clear the glucose. Eventually, our cells can start becoming resistant to insulin.
With elevated cortisol levels, the body also produces less testosterone, leading to a decrease in muscle mass, and your body starts burning fewer calories. This can lead to the dreaded belly fat.
Additionally, chronic stress can have an immense impact on the proper functioning of the gastrointestinal system, as it alters the composition of the gut microbiome (dysbiosis), reduces gastrointestinal secretions, increases inflammation, and modifies the mucosal immune response.
In fact, studies have shown that 50–90% of IBS patients have associated psychiatric comorbidity. According to systematic review and meta-analysis, patients with IBS have a three-fold increased odds of either anxiety or depression, compared to healthy subjects.
This increased permeability of the gut barrier, as well as the stress-induced changes in the gut microbiota, can also influence the immune response in a way that eventually trigger an attack of the body, causing the development of various autoimmune diseases.
So all these various outcomes caused by a poor response to stress (insulin resistance, weight gain, abdominal fat, dysbiosis, inflammation, and immune activation) can lead to type 2 diabetes, as well as increase the risk for cardiovascular disease, stroke and a host of gastrointestinal, neurological, and autoimmune diseases.
The more research that is done, the more fundamental examples of the connection between the mind, gut and disease continue to be seen.
Studies have also found that mind-body medicine is associated with an appreciable decline in symptom severity in conditions like IBS (irritable bowel syndrome), with improved quality of life and overall pain management also being seen in IBD (inflammatory bowel disease) and other autoimmune diseases.
This highlights the importance of mind-body medicine playing an important role in the treatment of numerous diseases, especially for those patients who have not had favorable outcomes with conventional medical management. These techniques may also help to reduce the global burden of disease associated with these conditions.
The Power Of Positive Thinking, The Placebo Effect, And The Vagus Nerve
We have already seen that your inner world can deeply affect all aspects of your physical health, including digestive function, immune system, hormone balance, and so on.
Science has shown that having a positive mindset makes for better health or at least helps you cope better and improves treatment compliance. A 2012 study found that people who thought of something that made them feel good each morning and used self-affirmation techniques when facing challenges were better at complying with their treatment plan.
The placebo effect is a phenomenon that highlights the value of positivity.
The placebo effect—when a bogus treatment in a scientific study produces the desired results—seems to work best when an individual’s beliefs and expectations about treatment are positive.
For example, in a 2011 study, researchers found that the participants’ perception of pain dropped significantly when they were told they received more of an analgesic (pain-relief) drug than they actually did. Having a positive expectation of the treatment considerably enhanced (doubled) the analgesic benefit of the drug. In contrast, those who were told the medication had stopped, reported higher levels of pain. The positive expectancy effects were associated with activity in the endogenous pain modulatory system, and the negative expectancy effects with activity in the hippocampus. The researchers concluded that integrating patients’ beliefs and expectations into drug treatment regimens can help optimize treatment outcomes.
In other words, your treatment has a much higher chance of being effective if you have a positive belief in it. Likewise, if you don’t think anything will work for you, you can negatively impact its chance of success.
This positivity effect is largely due to the role of the vagus nerve. The vagus nerve is the primary pathway that the gut and brain communicate through and it controls our inner nerve center—the parasympathetic nervous system. It is key in regulating the HPA axis pathway, a hormone pathway which controls our response to stress. It also communicates with the diaphragm to promote deep breathing, helping you become more relaxed. The vagus nerve regulates components of the gastrointestinal system and is also essential for regulating your immune system and inflammation.
Damage or impairment of the vagus nerve has been linked to major depression, PTSD, severe anxiety and inflammatory gastrointestinal disorders, including ulcerative colitis and Crohn’s disease.
In recent years, the vagus nerve has taken center stage as a potential “off switch” for not only treating psychiatric and gastrointestinal disorders but also a range of inflammatory diseases, such as rheumatoid arthritis, chronic headaches, fibromyalgia, and diabetes.
How You Can Cultivate a Positivity Habit
For those struggling with serious and debilitating health conditions, being told to “be positive” can be infuriating.
When fatigue has you feeling like every small task is a marathon and even getting up in the morning is the biggest achievement of your day, someone telling you to be positive can be dismissive and disparaging.
Positive thinking doesn’t mean you only ever experience rainbows and sunshine. It doesn’t mean you have to reject or suppress your negative emotions or that you can’t stay in bed on the days that you feel awful.
But there are things that anyone can do to cultivate a positivity habit. Research has shown that even just a few minutes a day of positive thinking can improve your health. Being positive is not just an ability one has or doesn’t have. It’s something you learn, just like learning a language or playing an instrument. It’s something you need to practice and cultivate.
Here are some mind-body techniques that you can employ to cultivate this positive outlook in order to enhance your treatment outcomes.
1. Practice gratitude
One of the best things you can do to start cultivating this habit of positivity is to practice gratitude. A grateful outlook has been linked to less anxiety and depression, better sleep, kinder behavior, and overall better health. It sends signals of safety to the brain, which, in turn, prompts the body to relax.
A study performed by The National Institute of Health in the US used MRIs (Magnetic Resonance Imaging) to show that subjects who practiced gratitude had an increase in blood flow to the hypothalamic region of their brain. Enhanced activity in this brain region inhibits cortisol, known to increase heart rate, blood pressure, and inflammation.
By keeping a gratitude journal where you write three to five things you are grateful for every day (or doing another practice of gratitude that suits you better), you can build more pathways in your brain for positivity until it becomes a habit. Making this practice part of your routine the same as brushing your teeth or taking a shower will help to solidify these neural pathways and better support your overall health.
2. Find your life’s purpose
Living a life without meaning or purpose can raise stress levels, promote depression, perpetuate inflammation, and foster chronic disease.
For example, on postmortem examination, brain autopsies of individuals who felt that they had purpose and meaning in their lives showed that they all exhibited markers of Alzheimer’s disease. However, the study showed that the participants who reported high levels of purpose in life exhibited better cognitive function despite the burden of the disease. Higher levels of purpose in life also reduced the effect of pathologic changes on cognitive decline. In other words, many of these individuals—thanks to the cognitive benefits of a meaningful, purpose-driven life—lived free of the symptoms of dementia, despite physically exhibiting markers of the disease on post-mortem examination.
3. Visualize positive outcomes constructively
Studies have shown that time spent visualizing better outcomes in a constructive way rather than simply fantasizing, increases your chances of a positive outcome.
For example, in one study, participants who spent a few minutes each day visualizing when, where, and how they were going to study for a test, performed better than those who simply visualized what it would feel like to get a good grade.
The same held true when similar studies were done on tennis and golf players. Those who visualized practicing performed better than those who visualized winning. To apply it to being healthy, it’s better to visualize practices such as exercising, meditating, going to bed on time, and cooking healthy food, rather than just simply imagining how good it would feel to be healthy.
4. Surround yourself with positive people
While your own positivity is important for better health outcomes, so is the attitude of the people you connect with on a daily basis. Research shows that even having a positive and supportive health practitioner is going to influence the degree of improvement in your health.
The vagus nerve (the main nerve that connects your gut to your brain) responds to human connectivity and physical touch to activate the parasympathetic nervous system, which increases oxytocin and decreases cortisol. Studies have also linked a healthy social life with better heart health and the prevention of depression and memory loss.
Conversely, being socially isolated is so detrimental that it has been found to carry the same health risks as smoking, obesity, and lack of physical activity, while regular social connection can increase your likelihood of survival by 50%.
Unhealthy relationships can also be injurious to your health. Research has shown that it is better to be alone than to experience the negativity of destructive relationships, which increases stress and depression.
Therefore, it’s important to spend quality time with positive people as much as possible. If you don’t have great social or support networks around you, look online to find Facebook groups that you can connect with in person, join a club or sporting activity, or even reach out to your neighbors.
5. Embrace healthy touch
Research has shown that regular healthy touch, whether from loved ones or through manual therapy like a massage has been shown to improve immune function and promote good cardiovascular health. It helps to lower cortisol, stimulate the release of oxytocin, slow the heart rate, lower blood pressure, and decrease inflammation—all of which enable better functioning of the immune system.
6. Laugh often
When someone says “laughter is good medicine,” they’re not lying. This is because laughter stimulates the vagus nerve and releases endorphins that help you to stay calm, think clearly, and make better decisions. Studies have shown that laughter improves immunity, decreases stress, helps regulate blood sugar, alleviates depression and anxiety, increases pain tolerance, and improves your sense of well-being.
7. Bring play back into your life
As we get older, we often lose the ability to play. However, play is another way to develop a sense of positivity for better health. In fact, all animals continue to play throughout their lifespan, except perhaps, for many human adults. Play helps to reduce cortisol, form social connections, provide healthy stimulation for the brain, and create happiness and positivity. Play should be purposeless and fun. Some playful activities you can incorporate include playing with your dog or children, roller blading, swimming, skipping, or participating in a sport for fun.
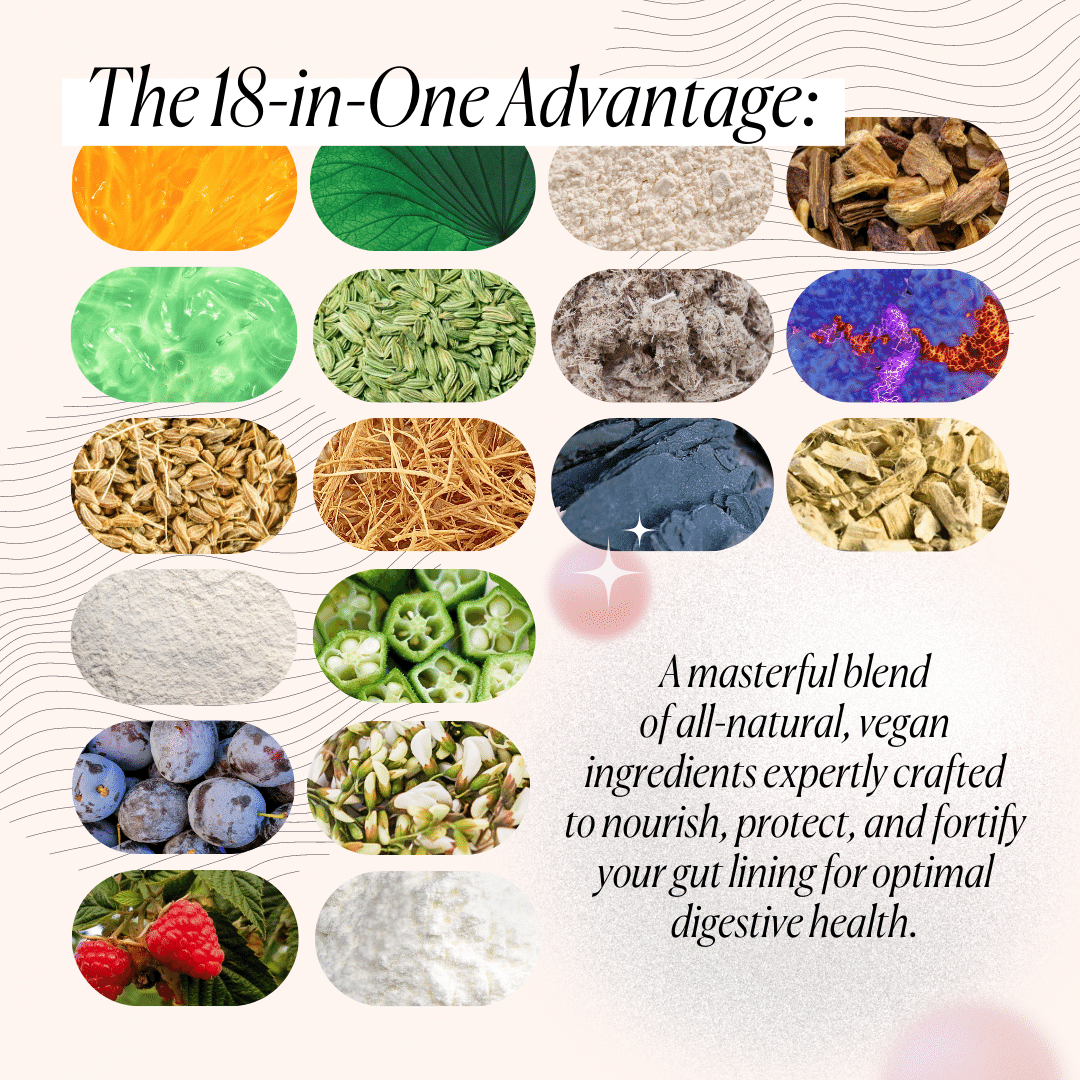
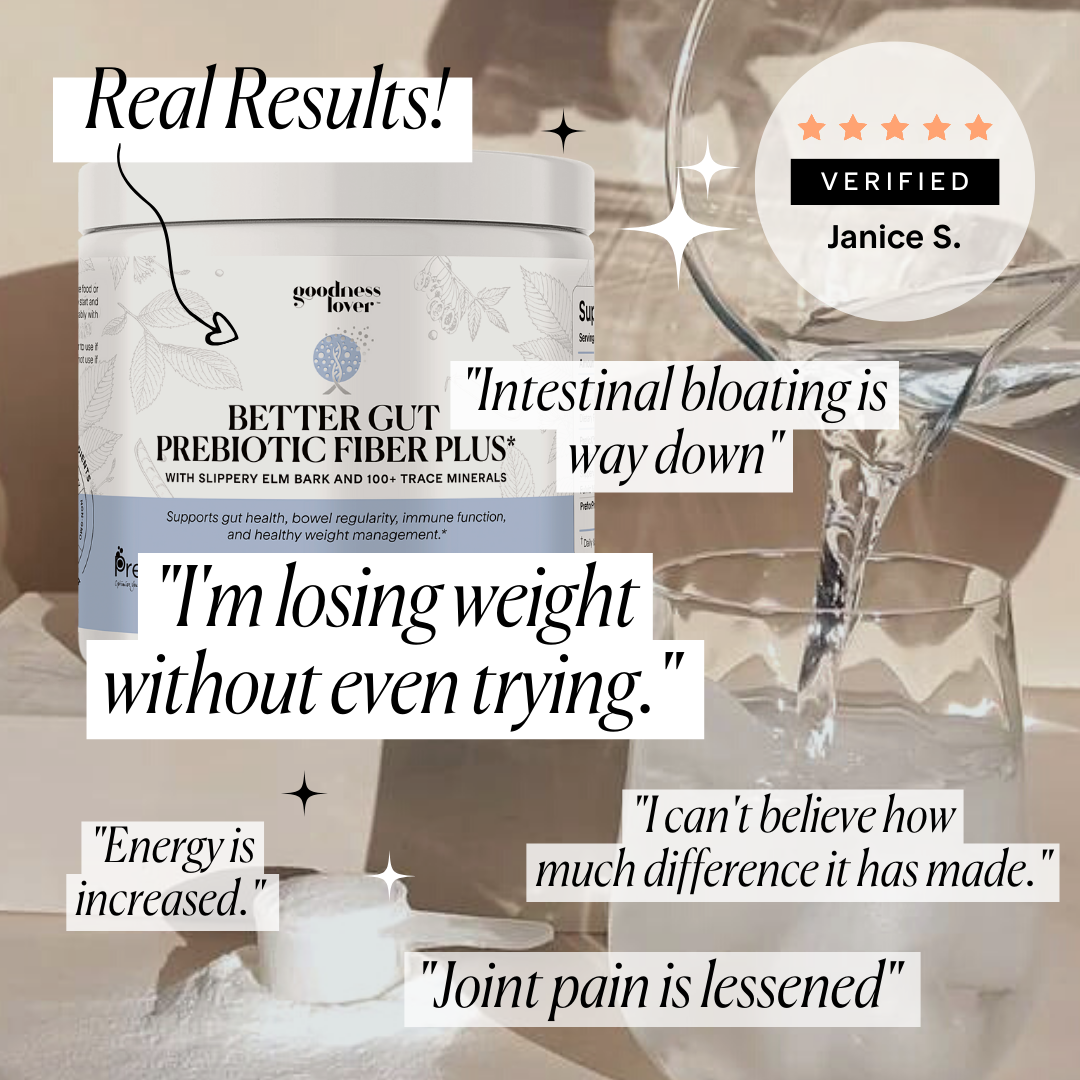
8. Supporting positivity with supplements
Herbs and nutrients have been used medicinally for thousands of years to promote a more positive frame of mind.
For example, 5-hydroxytryptophan (5-HTP) is a supplement used to boost serotonin (our happy hormone) activity. Depression has been associated with low serotonin levels and studies have shown that 5-HTP works better than placebo at alleviating depression.
L-theanine—an amino acid that elevates levels of GABA, our calming neurotransmitter—has been shown to reduce stress-related symptoms such as depression, anxiety, and sleeplessness.
Probiotics can also be utilized to assist the mind-body connection. Research has shown that probiotic therapy reduces depressive symptoms and improves the stress response as effectively as Citalopram or Diazepam, two very common antidepressant and anti-anxiety medications. In a 30-day study, healthy volunteers with no previous depressive symptoms were given either probiotics or antidepressants. Those given probiotics showed reduced cortisol levels and improved self-reported psychological effects to a similar degree as participants who received Diazepam.
Particular probiotic strains may also influence vagal nerve tone. Studies have demonstrated probiotics can cause alterations of both the gut microbiota and vagal tone in patients with depression, anxiety, and schizophrenia. Some probiotics, such as Bifidobacterium, signal to the brain via vagal pathways. In clinical studies where animals were supplemented with Lactobacillus rhamnosus showed alterations in GABA receptors that were mediated by the vagus nerve.
Finally, choline is another supplement that can help improve vagal tone, reduce inflammatory cytokines and improve memory and focus. It is the precursor to acetylcholine (ACh) which is involved in numerous key reactions including muscle control, memory and mediation of emotion and behavior in the brain, all due to its effects on the vagus nerve.
Animal studies have shown that choline ameliorates cardiovascular damage by improving vagal activity and inhibiting the inflammatory response, showing promising benefits for therapeutic use in other inflammatory conditions such as depression.
Future Directions
So how exactly do happiness, positivity, and socialization improve health?
They profoundly influence stress levels, inflammation, vagal tone, and the release of feel-good chemicals—all of which play roles in the treatment and prevention of disease. Negative thought patterns, social isolation, toxic relationships, living a life without meaning or purpose—all these factors raise stress, perpetuate inflammation, and foster chronic disease.
The development of new fields of research including psychoneuroimmunology and psychoneuroendocrinology highlights the critical link between the gut, the brain, and our overall health, and the need for mind-body medicine to play a principal role in the management of disease.
Recipe Spotlight: Chia Crispbread
Are you one of the people who feel genuine joy when they’re moving around the kitchen? Or are you the type who prefers quick prep and cooking time so you can enjoy your food asap?
Regardless of your style, cooking can also help you cultivate a positivity habit. This can be a time for you to focus on your senses—whether it’s observing the colors of the ingredients in front of you or basking in the scents around you. Feel grateful for the home-cooked meal that you’re about to eat.
And here’s another thing to feel grateful for today: Our chia crispbread recipe removes all the harmful ingredients from your regular store-bought bread, so you can still eat it without worrying about introducing more yeast into your body. Perfect if you’re trying to beat candida overgrowth, a condition that’s harmful to your gut.
Enjoy!











What Do You Think? Comment Below: